Low back discomfort is one of the most common complaints in today’s busy world, yet its source is not always easy to pinpoint. For many, persistent pain isn’t due to a simple muscle strain or a herniated disc but may actually originate from a less obvious culprit: the sacroiliac (SI) joint. In this post, we’ll explore how instability in this small yet essential joint can lead to significant pain, unraveling its complex anatomy, common symptoms, underlying causes, and the latest treatment options—all explained in straightforward, everyday language.

Understanding the Sacroiliac Joint
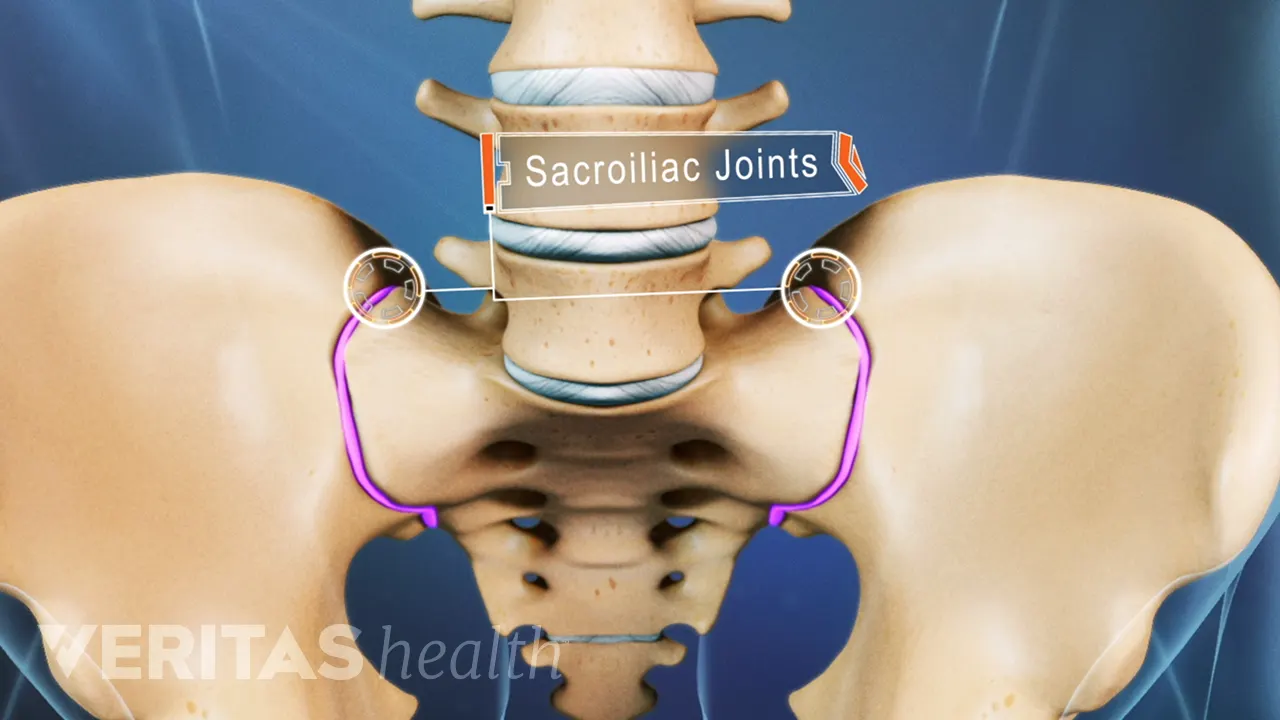
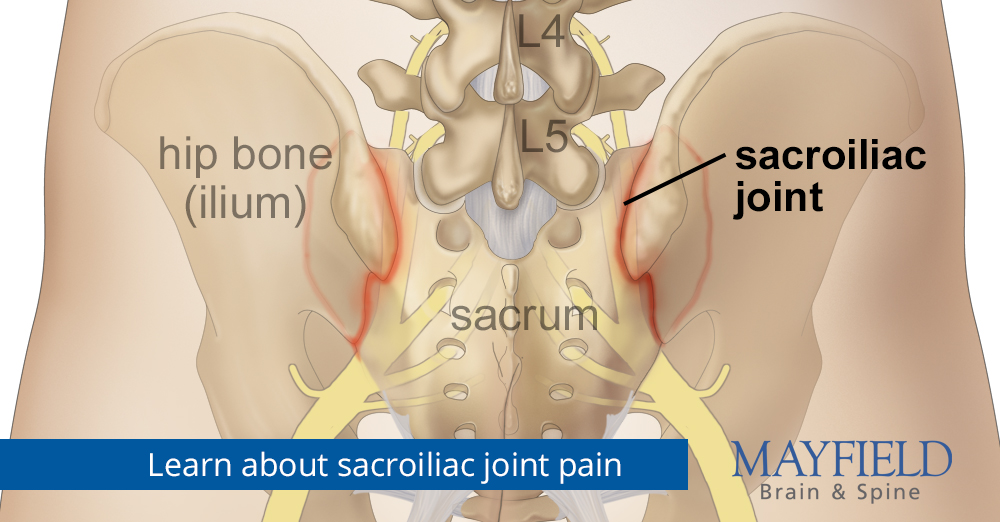
The sacroiliac joints are the key connectors between your spine and pelvis. These paired joints, found on either side of your lower back, serve as shock absorbers, transferring the weight of your upper body to your hips and legs as you move. Despite their small size and limited range of motion, they play a critical role in stability and movement. When the natural alignment or function of these joints is compromised, the result can be persistent pain that radiates through the lower back, hips, buttocks, and even the legs.
Anatomically, the SI joint is where the triangular sacrum meets the ilium—the large, wing-like bones that form your pelvic structure. This joint is held together by strong ligaments that help maintain its stability. However, when these ligaments are weakened or overly stretched, the joint can become either too loose (hypermobility) or too restricted (hypomobility). Both scenarios lead to what is broadly known as SI joint instability, a condition that many healthcare providers agree can be a significant source of chronic pain. For a detailed anatomical overview, you might explore resources from Cedars Sinai.
What Is SI Joint Instability?
At its core, SI joint instability refers to the joint’s inability to maintain its proper range of motion. Think of it like a door hinge that is either too loose or stuck—it simply can’t function as intended. In the case of the SI joint, instability may manifest as:
- Hypermobility (Excessive Movement): When the ligaments become too loose, the joint may move beyond its normal limits. This can lead to abnormal stress on the joint surfaces and the surrounding tissues, resulting in pain and inflammation.
- Hypomobility (Restricted Movement): Conversely, if the joint becomes too stiff or “locked,” often due to degenerative changes or fixation, the lack of proper movement can also trigger pain.
Both forms of instability disrupt the normal biomechanical functions of the pelvis and lower back, contributing to a cascade of discomfort that can affect your daily activities.
Recognizing the Symptoms
Identifying SI joint instability can be challenging because its symptoms often mimic other common conditions like sciatica or lumbar disc issues. However, there are specific signs that can help you suspect that your pain may be originating from the SI joint:
- Localized Pain: A dull, aching, or sharp pain in the lower back, buttocks, or hips that may radiate to the groin or upper thigh. Unlike typical sciatica, which often causes more pronounced leg weakness, SI joint pain is more about a persistent ache that worsens with movement.
- Movement-Triggered Discomfort: You might notice increased pain when transitioning from sitting to standing, climbing stairs, or during prolonged periods of standing or sitting. The pain may feel more pronounced on one side, particularly if one SI joint is more affected than the other.
- Stiffness and Instability: Many individuals report a sensation of stiffness in the pelvic area, sometimes even feeling that one leg is shorter or that their hips are misaligned. This sensation of instability may also be accompanied by a burning feeling in the lower back.
- Referred Pain: It is not uncommon for the pain to extend beyond the SI joint region. In some cases, the discomfort can radiate down the back of the leg, creating a pattern similar to sciatica, which can be misleading. For a patient-friendly explanation of these symptoms, check out insights from Spine Connection.
Underlying Causes and Risk Factors
The causes of SI joint instability are multifaceted, and several factors may contribute to its development. Here are some of the most common culprits:
- Trauma and Injury: Accidents, falls, or high-impact injuries can disrupt the normal functioning of the SI joint. Even repetitive microtrauma—such as that experienced by athletes—can lead to ligamentous strain and joint instability.
- Pregnancy and Childbirth: During pregnancy, hormones like relaxin increase ligamentous laxity to allow the pelvis to expand for childbirth. This temporary state of hypermobility can sometimes persist long after delivery, resulting in chronic instability.
- Degenerative Changes: As we age, wear and tear on the joints can lead to conditions like osteoarthritis. Degenerative changes in the cartilage and ligaments surrounding the SI joint can reduce its stability and function.
- Abnormal Gait or Leg Length Discrepancy: Even subtle differences in leg length or an altered walking pattern can place uneven stress on the SI joint, gradually contributing to its dysfunction.
- Previous Surgeries: Procedures such as lumbar fusion can increase stress on the adjacent SI joints, potentially leading to instability over time.
Understanding these risk factors can help you recognize whether your lifestyle or history might be contributing to your pain. For further reading on the impact of these factors, see the detailed explanation provided by Mayo Clinic.
Diagnosing SI Joint Instability
One of the biggest challenges with SI joint instability is that it often masquerades as other types of low back pain. This similarity means that an accurate diagnosis typically requires a comprehensive evaluation by a skilled healthcare provider. The diagnostic process may include:
- Medical History and Physical Exam: A thorough discussion of your symptoms and a detailed physical examination are critical. Your doctor will likely perform specific provocative tests—maneuvers designed to stress the SI joint—to see if they reproduce your pain.
- Imaging Studies: While standard X-rays, CT scans, or MRIs might not always reveal the subtle changes in the SI joint, they can help rule out other conditions such as herniated discs or fractures. Advanced imaging techniques, like SPECT-CT, have shown promise in highlighting mechanical abnormalities within the joint.
- Diagnostic Injections: One of the most definitive ways to determine if the SI joint is the pain generator is by injecting a local anesthetic directly into the joint. A significant reduction in pain following the injection confirms that the SI joint is likely responsible. To learn more about this diagnostic approach, you can explore resources from Weill Cornell.
Because no single test is foolproof, doctors often use a combination of these methods to arrive at a clear diagnosis. Recognizing SI joint instability early on is crucial, as it opens the door to more targeted and effective treatments.
Treatment and Management Options
Once SI joint instability has been diagnosed, a wide range of treatment options is available, tailored to the severity of the condition and your individual needs. The approach typically starts with conservative measures and may progress to more advanced interventions if needed.
Conservative Therapies
For many patients, non-surgical treatments provide significant relief and help restore function. These options include:
- Physical Therapy: Targeted exercises are designed to strengthen the core muscles, improve pelvic stability, and correct imbalances. A well-rounded physical therapy program often focuses on stretching tight muscles and reinforcing weak ones, such as the gluteal muscles and the deep abdominal muscles like the transversus abdominis. Resources like Spine-health offer detailed exercise routines and tips.
- Chiropractic Manipulation: In some cases, manual adjustments performed by a qualified chiropractor or osteopathic physician can help improve joint mobility and reduce pain.
- Medications: Over-the-counter pain relievers, such as nonsteroidal anti-inflammatory drugs (NSAIDs), can help reduce inflammation and manage discomfort.
- Injections: Corticosteroid injections into the SI joint may provide temporary relief by reducing inflammation. These injections not only help manage pain but can also serve as a diagnostic tool. For more on injection therapies, check out the insights provided by Mayfield Clinic.
Minimally Invasive Procedures
If conservative measures fail to provide sufficient relief, more advanced interventions may be considered:
- Radiofrequency Ablation: This procedure involves using heat to disrupt the nerve signals that transmit pain from the SI joint. It is often recommended when patients experience temporary relief from diagnostic injections but continue to suffer chronic pain.
- SI Joint Fusion: In cases of severe instability, surgical fusion of the SI joint may be performed. Minimally invasive techniques have advanced significantly, resulting in reduced recovery times and lower risks compared to traditional open surgeries. For a deeper dive into fusion surgery, you can explore the detailed procedures outlined by OrthoIndy.
Regenerative Treatments
Emerging therapies, such as stem cell injections and platelet-rich plasma (PRP), are also gaining traction. These treatments aim to promote healing and regeneration of damaged tissues within the joint, potentially restoring stability without the need for more invasive surgery.
Exercises and Lifestyle Modifications
Beyond formal medical treatments, certain lifestyle changes and exercises can make a significant difference in managing SI joint instability. Here are some strategies that may help:
- Core Strengthening: Building a strong core is essential for supporting the SI joint. Incorporate exercises that target the deep abdominal muscles, such as planks and pelvic clock exercises, to enhance stability.
- Stretching and Flexibility: Regular stretching, particularly for the hip flexors, quadratus lumborum, and hamstrings, can alleviate tension around the joint. Maintaining flexibility helps reduce the abnormal stress on the SI joint.
- Postural Adjustments: Correcting poor posture and ensuring proper alignment when sitting, standing, or moving can significantly reduce the strain on your SI joint. Ergonomic adjustments at work and at home—such as using supportive chairs and taking frequent breaks to move—can be very beneficial.
- Targeted Exercises: Specific routines have been designed to help “reset” the SI joint. For example, gentle yoga stretches or low-impact activities like water therapy can improve circulation and promote healing without overloading the joint.
- Weight Management: Maintaining a healthy weight reduces the overall stress on your joints, including the SI joint. Even modest weight loss can improve symptoms in many patients.
For those looking for practical exercise programs and additional tips, the guidance provided by Pelvic Clock offers creative and effective routines aimed at stabilizing the SI joint.
Simplifying the Complex: How Instability Leads to Pain
One of the most confusing aspects of SI joint instability is understanding how a small joint can cause such widespread pain. Imagine the SI joint as a tiny hinge that, when it fails to function properly, sends shockwaves throughout your lower back and hips. When the joint moves excessively (hypermobility), the surrounding muscles and ligaments must work overtime to stabilize it, leading to inflammation and discomfort. On the other hand, if the joint is too stiff (hypomobility), the lack of normal movement can cause irritation and abnormal stress distribution across the pelvis.
This imbalance not only contributes to localized pain but can also alter your gait—how you walk—causing compensatory issues elsewhere in your body. Even subtle imbalances, such as a minor leg length discrepancy or poor posture, can have a ripple effect on your SI joint, gradually leading to chronic instability and pain. Simplifying this concept can help you appreciate why a multidisciplinary approach—combining physical therapy, lifestyle changes, and possibly interventional procedures—is often the most effective way to manage the condition.
When to Seek Professional Help
If you’ve been experiencing persistent low back or hip pain that doesn’t respond to standard treatments, it might be time to consider the possibility of SI joint instability. While the symptoms can be subtle and easily confused with other conditions, early diagnosis and treatment are key to preventing further deterioration and improving your quality of life.
A thorough evaluation by a specialist—a physical therapist, orthopedic surgeon, or pain management expert—can determine whether your pain is truly coming from the SI joint. These professionals use a combination of physical tests, imaging studies, and sometimes diagnostic injections to pinpoint the source of your discomfort. For example, the evaluation techniques described by NCBI offer a comprehensive approach to differentiating SI joint pain from other types of low back pain.
Integrating New Technologies and Techniques
Advancements in medical technology have significantly improved the diagnosis and treatment of SI joint instability. Minimally invasive procedures, in particular, have revolutionized patient care by offering effective pain relief with shorter recovery times. For instance, SI-BONE’s approach to diagnosing and treating sciatica that originates from the SI joint highlights how precision-guided interventions can offer long-term relief for patients who have struggled with chronic pain.
Additionally, regenerative therapies such as PRP and stem cell injections are emerging as promising options. These treatments aim not only to reduce inflammation but also to repair damaged tissues, potentially restoring stability to the SI joint. Although these approaches are still under study, many patients have experienced significant improvements in pain and function through these innovative treatments.
A Personal Perspective on Living with SI Joint Instability
Living with SI joint instability can be a frustrating and life-altering experience, especially when traditional treatments fail to provide lasting relief. Many individuals find that the pain disrupts everyday activities—from sitting at a desk to enjoying a leisurely walk—and can even impact sleep quality. However, understanding the root cause of the pain is the first step toward effective management and recovery.
For those who have navigated this challenging journey, integrating a combination of targeted physical therapy, lifestyle modifications, and, when necessary, minimally invasive procedures has often proven transformative. By focusing on building core strength, maintaining proper posture, and staying active, many patients have regained their quality of life and reduced their reliance on pain medications.
Conclusion
Sacroiliac joint instability is a complex condition that often hides behind common symptoms of low back pain. With its origins in the delicate balance between stability and mobility in the SI joint, this condition can lead to widespread discomfort that affects your entire lower body. Yet, with a comprehensive understanding of the joint’s anatomy, awareness of the potential causes, and a multifaceted approach to treatment, it is possible to manage—and even overcome this challenging source of pain.
If you suspect that your pain may be rooted in SI joint instability, it’s important to seek a thorough evaluation from a knowledgeable specialist. With advancements in diagnostic imaging, minimally invasive procedures, and regenerative therapies, there are more options than ever before for restoring stability and alleviating pain. Remember, effective treatment is not one-size-fits-all; it involves a tailored approach that considers your unique body mechanics, lifestyle, and overall health.
Ultimately, understanding and addressing SI joint instability is a journey—a process that involves not only medical intervention but also lifestyle changes and active participation in your own recovery. By staying informed and proactive, you can take charge of your pain and work toward a more comfortable, active life.
The information presented in this article is intended for educational purposes only. It is not meant to replace expert consultation or a personalized treatment plan.
Sources: