Rheumatoid arthritis is more than just joint pain—it’s an inflammatory condition where the body’s immune system mistakenly attacks its own tissues, primarily targeting the joints. This attack results in inflammation, pain, swelling, and eventual joint damage if left untreated. Unlike osteoarthritis, which is primarily caused by wear and tear, RA is an autoimmune disorder that can affect the entire body, sometimes manifesting in systemic symptoms like fatigue and fever. According to the NHS, RA symptoms typically evolve gradually, although in some cases the progression can be much faster.
The complexity of RA means that its symptoms are not static. Many patients report that their joints feel particularly stiff in the morning, sometimes lasting more than an hour, and then improve as the day goes on. However, a subset of individuals experiences significant pain at night, which can interfere with sleep and overall well-being. Both patterns—the prolonged morning stiffness and the persistent night pain—reflect the dynamic interplay of immune system activity, hormonal fluctuations, and other factors that are tightly linked to the body’s internal clock.

The Circadian Connection: Why Mornings are So Stiff
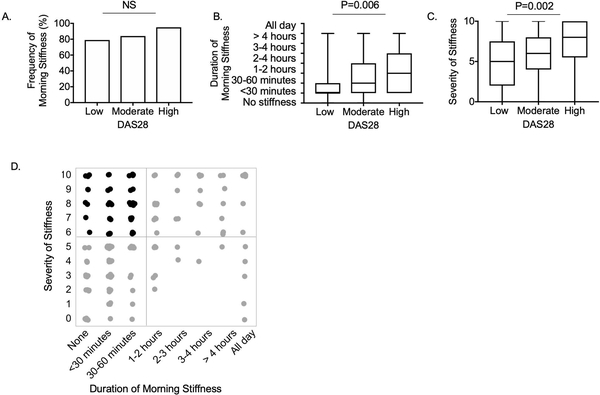
One of the most intriguing aspects of rheumatoid arthritis is how it is affected by the body’s circadian rhythms—the natural, internal process that regulates the sleep-wake cycle over a 24-hour period. Research from the PMC suggests that key inflammatory markers and histologic features, such as fibrin deposits and neutrophil infiltration in the synovial lining, are associated with the duration and severity of morning stiffness. During sleep, the joint tissues are relatively inactive, and over time, inflammatory mediators can accumulate, leading to the “gel phenomenon.” In this state, synovial fluid thickens, making joints feel stiff and less lubricated upon waking.
Additionally, hormone fluctuations play a crucial role. Cortisol, a hormone with potent anti-inflammatory properties, peaks in the early morning. Yet paradoxically, many RA patients still experience significant stiffness at this time. This discrepancy may be due to a lag in the cortisol effect or an overwhelming inflammatory process that outpaces the hormone’s natural anti-inflammatory action. As the day progresses and movement increases, joint fluids redistribute and the inflammatory response often subsides, leading to improved mobility. The research outlined by Harvard Health explains that these natural rhythms mean that the body’s capacity to counter inflammation is not constant throughout the day.
When RA Keeps You Awake?
While morning stiffness is a well-documented symptom, many people with RA also struggle with pain during the night. Night pain can be just as debilitating as morning stiffness, impacting sleep quality and overall health. Several factors contribute to this phenomenon:
- Inflammatory Activity: Inflammatory processes are not confined to the morning. Some individuals may experience an increase in inflammatory cytokines during the night, which can lead to persistent pain. The exact triggers for this nocturnal inflammation are still under investigation, but they are believed to be related to the body’s internal clock and the cyclical release of various hormones.
- Joint Lubrication and Fluid Dynamics: Just as synovial fluid can thicken during periods of inactivity at night, its viscosity may contribute to discomfort when a person first moves upon waking. This effect can be compounded if there is underlying joint damage or if the inflammatory process has been particularly active during the night.
- Sleep Disturbances: Poor sleep quality can exacerbate pain. When the body is deprived of restorative sleep, the perception of pain can be heightened. Chronic sleep disruption is known to lower the pain threshold, meaning that even normal levels of inflammation might feel more intense. The WebMD resource highlights that a disrupted sleep cycle often results in heightened pain sensitivity, further complicating the management of RA symptoms.
In essence, night pain in RA is a multifaceted problem, stemming from both biological processes and lifestyle factors. Understanding the interplay between these elements is key to developing effective management strategies.
Underlying Mechanisms of RA
To simplify the science behind RA symptoms, it is helpful to break down the processes into a few core components:
- Inflammation and Immune Response: At its core, RA is an autoimmune disease. The immune system mistakenly identifies joint tissues as foreign invaders, launching an inflammatory response. This response involves a host of cells—including neutrophils and other white blood cells—that release inflammatory cytokines. These cytokines not only cause pain and swelling but also contribute to the formation of fibrin deposits, which have been linked to prolonged morning stiffness (PMC).
- Circadian Hormonal Fluctuations: The body’s natural rhythms affect the production and release of hormones such as cortisol and melatonin. Cortisol, which is anti-inflammatory, is highest in the early morning, yet its effects might be insufficient to fully counteract the inflammation built up overnight. Melatonin, on the other hand, peaks at night and may even exacerbate inflammation, further contributing to night pain. These hormonal oscillations mean that the inflammatory process in RA is highly time-dependent.
- Synovial Fluid Dynamics: The synovial fluid that lubricates joints can change in consistency based on activity levels. During periods of rest—whether overnight or during long stretches of inactivity—the fluid can become more viscous. This thickening can lead to increased friction and stiffness, making joints feel “frozen” until they are warmed up by movement.
- Structural Joint Changes: Over time, chronic inflammation can lead to physical changes in the joints, including erosion of cartilage and bone, and the development of rheumatoid nodules. These structural changes can exacerbate symptoms and alter the pattern of pain throughout the day.
By understanding these mechanisms, it becomes easier to see why RA symptoms can vary so much not only between different people but also within the same individual at different times.
Differentiating RA from Other Forms of Arthritis
A significant challenge in managing arthritis is distinguishing RA from other types of joint disorders, particularly osteoarthritis (OA). While both conditions cause joint pain and stiffness, there are important differences:
- Onset and Progression: Osteoarthritis is primarily a degenerative condition caused by wear and tear on the joints. It tends to develop gradually over many years and usually affects weight-bearing joints like the knees and hips. In contrast, RA can occur at any age, often with a more rapid onset, and typically affects smaller joints symmetrically (as noted by MyHealth.Alberta).
- Stiffness Duration: Morning stiffness in OA generally lasts less than 30 minutes, while RA-associated stiffness is usually prolonged, often exceeding one hour. This distinction is a useful diagnostic clue for physicians.
- Systemic Symptoms: RA is a systemic disease. Beyond joint pain, it can cause fatigue, low-grade fever, and a general feeling of malaise. Osteoarthritis, on the other hand, is confined largely to the joints without these systemic effects.
- Inflammatory Markers: Laboratory tests can also help differentiate the two. RA is typically associated with elevated inflammatory markers and the presence of specific autoantibodies, such as rheumatoid factor (RF) and anti-citrullinated peptide antibodies (ACPA) (UpToDate).
Understanding these differences not only aids in accurate diagnosis but also ensures that treatment strategies are appropriately tailored to the specific condition.
Treatment Strategies
Managing the fluctuating symptoms of rheumatoid arthritis involves a multi-pronged approach. Treatments focus on reducing inflammation, relieving pain, and preserving joint function. Here are some key strategies:
Medications and Medical Treatments
Disease-modifying antirheumatic drugs (DMARDs) and biologics are the cornerstone of RA management. These medications work by dampening the immune response, thereby reducing inflammation and slowing the progression of joint damage. Nonsteroidal anti-inflammatory drugs (NSAIDs) and corticosteroids are often used to manage acute symptoms. The Cleveland Clinic emphasizes that timely and effective medication can not only alleviate pain but also help maintain a more active lifestyle.
Chronotherapy: Aligning Treatment with the Body’s Clock
An emerging field in RA treatment is chronotherapy, which involves timing the administration of medications to coincide with the body’s natural rhythms. Since inflammation peaks at certain times of the day—often in the early morning—taking medications at night can help mitigate the morning stiffness. For instance, delayed-release prednisone taken around 10 p.m. can be particularly effective by ensuring that anti-inflammatory levels are high when symptoms are likely to peak (Versus Arthritis).
Lifestyle Adjustments and Physical Therapies
Exercise is a powerful tool in managing RA symptoms. Gentle stretching, range-of-motion exercises, and activities like walking or swimming can help increase joint lubrication and reduce stiffness. Heat therapy, such as a warm shower or using a heating pad, can also relax muscles and ease pain. Resources from WebMD suggest that even a short period of physical activity can break the cycle of stiffness and improve overall joint function.
Sleep hygiene is another important aspect. Given that both inadequate sleep and sleep disturbances can exacerbate pain, establishing a consistent sleep routine is essential. Creating a comfortable, dark, and quiet sleeping environment, while also managing pain before bedtime with appropriate medication or heat therapy, can lead to more restorative sleep and reduce night pain.
Diet and Nutrition
Emerging research indicates that certain dietary choices can influence inflammation. A diet rich in anti-inflammatory foods—such as fruits, vegetables, whole grains, and omega-3 fatty acids—may help reduce systemic inflammation. Some studies even suggest that maintaining a healthy weight can lessen the stress on joints, particularly in weight-bearing areas, further alleviating pain (Harvard Health).
Practical Tips for Managing RA Symptoms Throughout the Day
Living with rheumatoid arthritis means adapting daily routines to minimize discomfort and maintain functionality. Here are several practical strategies:
- Morning Routine: Begin the day slowly. Allow extra time in the morning to gently stretch and warm up the joints before jumping into daily activities. Consider taking a warm shower or using a heating pad immediately after waking to ease stiffness. Establishing a consistent morning routine can make the transition from sleep to wakefulness smoother.
- Medication Timing: Work with a healthcare provider to optimize medication schedules. Chronotherapy, where medications are timed to counteract peak inflammatory periods, has shown promising results. For many, taking certain medications at night can significantly reduce the severity of morning stiffness.
- Regular Exercise: Incorporate low-impact exercises into daily life. Even brief periods of gentle movement can help maintain joint mobility and reduce stiffness. Activities like yoga, swimming, or a short walk can make a noticeable difference in how the joints feel.
- Sleep Hygiene: Prioritize a good night’s sleep by creating an optimal sleep environment. Ensure that the bedroom is dark, cool, and quiet, and maintain a regular sleep schedule. If night pain is problematic, discuss with a healthcare provider about potential adjustments in pain management strategies before bedtime.
- Stress Management: Chronic pain and inflammation can be exacerbated by stress. Techniques such as meditation, deep breathing exercises, or maintaining a gratitude journal can help manage stress levels, thereby potentially reducing pain intensity.
- Diet and Hydration: Stay hydrated and choose a diet that supports joint health. Avoid foods that are known to trigger inflammation, and consider incorporating supplements like vitamin D if recommended by a doctor.
- Professional Support: Regular consultations with rheumatologists, physical therapists, and occupational therapists are crucial. These experts can provide personalized guidance on exercise, medication adjustments, and ergonomic modifications to reduce joint strain throughout the day.
The Science Behind Symptom Variation
The variations in symptoms between morning stiffness and night pain highlight the intricate balance between the body’s immune system and its circadian clock. During the night, the body’s metabolic and hormonal cycles set the stage for inflammation to build up. This is why many people with RA wake up with stiff, painful joints that gradually loosen with activity. Conversely, as the day goes on, increased movement and better circulation help clear inflammatory mediators from the joints, reducing stiffness and pain.
Recent research has even explored how certain cells in the joint lining, such as neutrophils, interact with fibrin—a protein involved in blood clotting—to form deposits that resist breakdown. These deposits can contribute to prolonged stiffness by physically hindering joint movement (PMC). Additionally, the fluctuating levels of hormones like cortisol and melatonin further complicate the picture. While cortisol should theoretically reduce inflammation, its effects can be offset by the overwhelming activity of inflammatory cells during the early morning hours.
Understanding these processes not only provides insight into why symptoms vary but also opens the door to more effective treatment strategies. By aligning medication schedules and lifestyle modifications with the body’s natural rhythms, patients can achieve better symptom control and a higher quality of life.
RA Isn’t One-Size-Fits-All
No two experiences with rheumatoid arthritis are exactly alike. Some people may find that their primary challenge is the debilitating stiffness that plagues their mornings, while others might struggle more with night pain that disrupts sleep and daily energy levels. This individuality means that treatment and management strategies need to be tailored to the person’s specific symptoms and lifestyle.
For instance, a patient who experiences severe morning stiffness might benefit from adjusting their sleep environment or shifting their medication timing to ensure that anti-inflammatory drugs are most effective during the early hours. On the other hand, someone troubled by night pain might need to explore different pain management techniques, such as targeted stretching before bed or the use of supportive devices to maintain proper joint alignment during sleep.
Consulting with healthcare providers who understand the nuanced nature of RA is essential. Whether it’s through a multidisciplinary team at a renowned center like the Johns Hopkins Arthritis Center or guidance from local specialists, personalized care can make all the difference.
Bridging the Gap Between Research and Daily Life
Recent studies have shed light on the cellular and molecular mechanisms that drive RA symptoms, yet translating these findings into everyday practices remains a work in progress. The evolving field of chronotherapy, for example, is a promising avenue that integrates our growing understanding of circadian biology with practical treatment regimens. Patients who adhere to a carefully planned medication schedule aligned with their natural biological rhythms often report a noticeable improvement in their morning symptoms, which underscores the potential of this approach.
Moreover, ongoing research continues to explore new therapeutic targets that might one day offer more precise control over the inflammatory processes that underlie both morning stiffness and night pain. While the science may be complex, the goal remains straightforward: to empower patients with strategies that allow them to reclaim control over their daily lives despite the challenges of RA.
Tips for Implementing Change
Adapting to life with rheumatoid arthritis involves more than just taking medication—it requires a holistic approach that encompasses physical, emotional, and lifestyle adjustments. Here are some actionable tips to help integrate these strategies into daily life:
- Establish a Consistent Sleep Schedule: Aim to go to bed and wake up at the same time every day. This consistency helps regulate the body’s circadian rhythms and can reduce the severity of morning stiffness. Consider using blackout curtains or a white noise machine to create an environment conducive to restful sleep.
- Plan a Gradual Morning Routine: Instead of jumping out of bed, take a few minutes to perform gentle stretches. Even a short period of light movement can help mobilize stiff joints and prepare the body for the day ahead.
- Optimize Medication Timing: Discuss with your doctor the possibility of taking certain medications at night rather than in the morning. This approach, as highlighted by Versus Arthritis, can ensure that anti-inflammatory effects peak when they are needed most.
- Incorporate Low-Impact Exercise: Regular, low-impact activities such as walking, swimming, or yoga can improve joint function and reduce stiffness. Even short bouts of exercise throughout the day can help maintain mobility.
- Stay Hydrated and Eat Nutritious Foods: Adequate hydration and a diet rich in anti-inflammatory foods can support overall joint health. Consider meals that include plenty of fruits, vegetables, lean proteins, and omega-3 fatty acids to help combat inflammation.
- Manage Stress Effectively: Stress can exacerbate RA symptoms, so adopting stress-reduction techniques—such as mindfulness meditation, deep breathing exercises, or even keeping a gratitude journal—can be beneficial. Engaging with supportive communities, whether online or in person, may also help alleviate the emotional burden of chronic illness.
- Seek Professional Guidance: Regular follow-ups with a rheumatologist and allied health professionals can ensure that treatment strategies remain effective and are adjusted as needed over time. Personalized care plans are key to managing a condition that can change from day to day.
Embracing a Flexible Management Plan
Living with rheumatoid arthritis is an ongoing journey of adaptation and learning. As research continues to evolve, the hope is that more targeted therapies and innovative management strategies will emerge. In the meantime, integrating current knowledge about the circadian influences on RA with practical lifestyle changes can make a significant difference.
Patients are encouraged to remain proactive in their care. This might mean experimenting with different exercise routines, adjusting medication timing, or exploring complementary therapies that help manage both physical and emotional symptoms. The ultimate goal is to create a flexible management plan that not only addresses the immediate challenges of morning stiffness and night pain but also enhances overall quality of life.
The Road Ahead
The variability in rheumatoid arthritis symptoms—whether it’s the prolonged stiffness of the morning or the persistent pain that can disrupt sleep at night—highlights the intricate interplay between the immune system, circadian rhythms, and lifestyle factors. By understanding these mechanisms and embracing personalized treatment strategies, it is possible to significantly alleviate the impact of RA on daily life.
Living with rheumatoid arthritis may be challenging, but with a proactive, flexible approach to managing symptoms, it is possible to find relief and maintain an active, fulfilling life. Whether it’s addressing the early morning stiffness or combating night pain, the key lies in understanding the underlying processes and tailoring management strategies accordingly. Embrace the journey toward better health—each step taken is a step toward a more comfortable and empowered life.
Sources: