Rheumatoid Arthritis: Take Control and Live Life to the Fullest
Struggling with rheumatoid arthritis? Discover expert tips and powerful strategies to reduce pain, improve mobility, and live your best life. Say goodbye to stiffness and hello to a more active, fulfilling lifestyle. Find out how to manage RA effectively in our ultimate guide!
Rheumatoid arthritis (RA) is a chronic autoimmune disease that affects your joints, but it's more than just joint pain. It’s a condition that can impact your entire body, and it tends to make daily activities harder to manage. If you’ve been diagnosed with rheumatoid arthritis, or you’re just trying to understand it better, this post will walk you through the basics and offer tips on how to manage the symptoms.
What Is Rheumatoid Arthritis?
Rheumatoid arthritis is a long-lasting, autoimmune disease that causes inflammation in the joints. This inflammation can lead to pain, swelling, and stiffness in the affected areas. Over time, if not treated, it may also cause damage to the bones and cartilage in the joints. While it commonly affects smaller joints like those in the hands and feet, it can impact larger joints as well, including the knees, shoulders, and elbows.
RA doesn’t just affect the joints—it’s a systemic disease, which means it can impact other parts of your body too. Many people with RA also experience fatigue, fever, weight loss, and general discomfort. In fact, the symptoms of RA can often be worse in the morning, with joint stiffness lasting for an hour or more.
How Does Rheumatoid Arthritis Affect the Body?
In simple terms, rheumatoid arthritis happens when your immune system, which is designed to protect you from infections, mistakenly attacks the lining of your joints. This lining, known as the synovium, becomes inflamed, thickened, and swollen. As a result, the cartilage and bones in the joint may start to break down, which can lead to deformities and loss of function in the joint.
The inflammation from RA can also affect other areas of the body. Over time, the damage to the joints may get worse, leading to permanent changes that can impact your movement and quality of life.
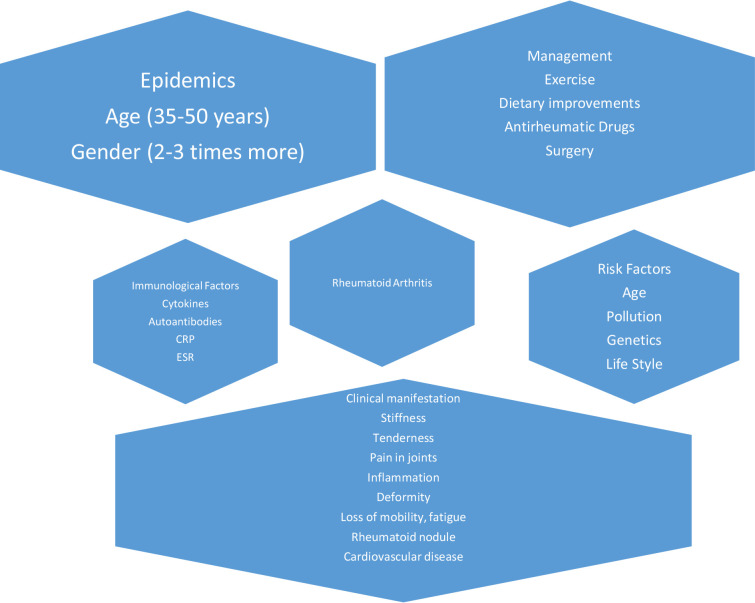
What Causes Rheumatoid Arthritis?
While the exact cause of rheumatoid arthritis is not fully understood, it’s believed to be a combination of genetic and environmental factors. If you have a family history of RA, your risk of developing it increases. But it's not just genetics—lifestyle factors like smoking, infections, and even diet can also play a role in whether or not you develop the disease.
Interestingly, RA is more common in women, possibly due to hormonal influences. Many women even notice that their symptoms change during pregnancy—sometimes they feel relief, but often symptoms flare up after giving birth.
Environmental Triggers
Certain environmental factors have been linked to the onset of rheumatoid arthritis. These include stress, infections, and even exposure to certain chemicals. While more research is needed to fully understand the links, it’s believed that these factors can trigger RA in people who are already genetically susceptible.

Symptoms of Rheumatoid Arthritis
Rheumatoid arthritis can start in a variety of ways, but it often begins with pain, swelling, and stiffness in the joints, especially in the hands, wrists, and feet. Over time, other joints, such as the elbows, knees, and ankles, may also be affected.
The disease is known for its "flare-ups," where symptoms worsen for a period before improving again. Common symptoms of RA include:
- Fatigue – Many people with RA experience extreme tiredness, even after a good night’s sleep.
- Low-grade fever – A mild fever is often present.
- Loss of appetite – People with RA often lose their desire to eat, which can contribute to weight loss.
- Rheumatoid nodules – These are small lumps that can form under the skin, usually near the elbows or hands.
- Joint pain and stiffness – The most noticeable symptom of RA, it’s often worse in the morning and can last for several hours.
In some cases, RA can also affect other organs, such as the eyes, lungs, and heart, leading to further complications.
How Is Rheumatoid Arthritis Diagnosed?
Rheumatoid arthritis is typically diagnosed through a combination of a physical exam, blood tests, and imaging tests. Doctors will look for signs of tenderness, warmth, or swelling in your joints. Blood tests can reveal markers of inflammation or the presence of specific proteins that are common in people with RA, such as rheumatoid factor and anti-CCP antibodies.
Imaging tests like X-rays or ultrasounds can show if there has been any joint damage and help track how the disease is progressing.
Treatment Options for Rheumatoid Arthritis
Although there is no cure for rheumatoid arthritis, there are several treatment options that can help manage the symptoms, slow the progression of the disease, and improve your quality of life. The goal of treatment is to reduce pain, minimize joint damage, and keep you as mobile and comfortable as possible.
Medications
A variety of medications are available to help treat RA. Some focus on reducing inflammation, while others aim to slow the disease’s progression.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications like ibuprofen and naproxen can help relieve pain and reduce inflammation in the short term.
- Steroids: Steroids such as prednisone are used to quickly reduce inflammation. They can be very effective during flare-ups but are typically prescribed for short periods due to their potential side effects.
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): These drugs work to slow the progression of RA and prevent further joint damage. Methotrexate is one of the most commonly prescribed DMARDs.
- Biological Agents: Biologics like etanercept and adalimumab target specific parts of the immune system to block the inflammatory process. These are often prescribed if other medications haven’t worked.
- Janus Kinase (JAK) Inhibitors: Newer oral medications, such as tofacitinib, block enzymes responsible for inflammation and are often used when other treatments aren’t effective.
Lifestyle Changes
Making lifestyle changes can help reduce the severity of rheumatoid arthritis and improve your quality of life. Exercise is important for keeping your joints flexible and strengthening the muscles around them. Low-impact activities like swimming, walking, or cycling are great options.
A balanced, anti-inflammatory diet rich in fruits, vegetables, and omega-3 fatty acids can also help reduce inflammation. Many people with RA find that certain foods can either ease or aggravate symptoms, so paying attention to how your body responds to different foods is key.
Surgery
In severe cases, surgery may be required. Joint replacement surgery can help restore function and relieve pain, particularly in the hips, knees, and shoulders.
Managing Life with Rheumatoid Arthritis
Living with rheumatoid arthritis can be tough, but it’s important to remember that you don’t have to face it alone. Many people with RA lead full, active lives with the right treatment and support. Working with your doctor to find the best treatment plan for your needs is essential, and there are resources like occupational therapy, physical therapy, and support groups that can help.
You may also find assistive devices, such as braces or specially designed tools, can make daily tasks easier. And remember, it’s okay to ask for help when you need it. Prioritize self-care and listen to your body.
Final Thoughts on Rheumatoid Arthritis
Rheumatoid arthritis can make life challenging, but it’s possible to manage the symptoms and live a fulfilling life with the right approach. From medications and physical therapy to lifestyle changes and emotional support, there are plenty of ways to take control of your health.
If you’re dealing with rheumatoid arthritis, start by talking to your doctor about the best treatment plan for you. Take small steps every day to stay active and healthy, and remember that you’re not alone—help is available.
Take Charge of Your Rheumatoid Arthritis Treatment
Dealing with rheumatoid arthritis can feel overwhelming, but the good news is that treatment options have come a long way. From medications to lifestyle changes, there's hope for improving your condition. If you’re struggling with symptoms, it’s time to talk to your healthcare provider about personalized treatments that can make a real difference.
Sources: