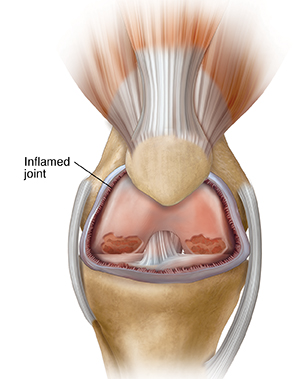
Psoriatic arthritis (PsA) is an autoimmune disorder characterized by the inflammation of joints and the skin. It typically occurs in people who have psoriasis—a condition marked by red, scaly patches and pitted nails. While psoriasis itself affects the skin, the joint inflammation seen in PsA can lead to significant discomfort and functional limitations. According to the Cleveland Clinic, PsA can present in a variety of ways: some patients experience mild joint discomfort, while others endure severe joint damage that may even result in deformities.
Unlike other forms of arthritis, psoriatic arthritis can involve asymmetrical joint pain, meaning that it might affect one side of the body more than the other. In addition to joint pain and swelling, patients may also experience morning stiffness, fatigue, and, in some cases, eye inflammation. Diagnosing PsA can be challenging because its symptoms overlap with those of other arthritic conditions, but early detection is crucial for effective management.

Causes and Underlying Mechanisms
While the exact causes of psoriatic arthritis remain under investigation, several factors appear to contribute to its development:
- Genetic Predisposition: A family history of psoriasis or arthritis increases the risk. Research shows that up to 40% of people with PsA have relatives with similar conditions.
- Immune System Dysregulation: PsA is classified as an autoimmune disease, where the immune system mistakenly attacks healthy tissues. This results in chronic inflammation affecting the joints and skin.
- Inflammatory Cytokines: Key players in the inflammatory process include cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin-17 (IL-17), and interleukin-23 (IL-23). These molecules trigger and sustain the inflammatory response, leading to joint damage and skin lesions. Insights from a MDPI study underscore how targeting these cytokines has become a cornerstone in developing effective therapies.
Understanding these mechanisms not only provides clarity on why the disease occurs but also paves the way for treatments that target specific components of the immune response.
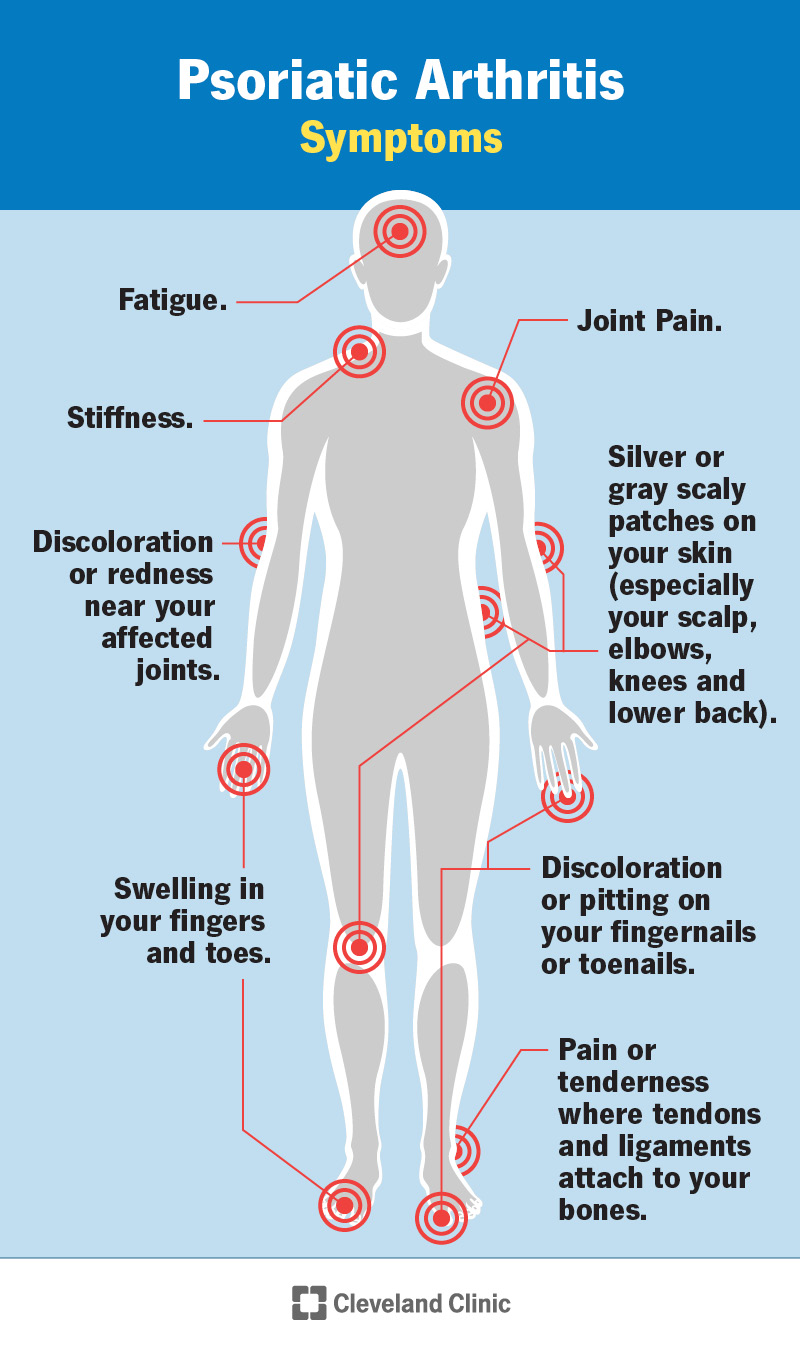
Recognizing the Symptoms and the Diagnostic Process
The early symptoms of psoriatic arthritis can vary widely between individuals, which sometimes delays diagnosis. Common symptoms include:
- Joint Pain and Swelling: Pain may occur in the fingers, toes, spine, or other joints. Swelling can be severe, sometimes causing a “sausage-like” appearance in affected digits.
- Stiffness: Particularly in the morning or after periods of inactivity.
- Nail Changes: Psoriasis often affects the nails, leading to pitting, thickening, or separation from the nail bed.
- Fatigue: Many patients report a persistent feeling of tiredness, which can significantly impact daily activities.
Screening tools such as the Psoriasis Epidemiology Screening Tool (PEST) are often used to identify PsA in patients with psoriasis. Detailed physical examinations, along with imaging studies like X-rays or ultrasound, help to assess joint inflammation and rule out other conditions. The NIAMS website provides further insights into the symptoms and diagnostic criteria used by healthcare professionals.
Treatment Approaches: An Overview
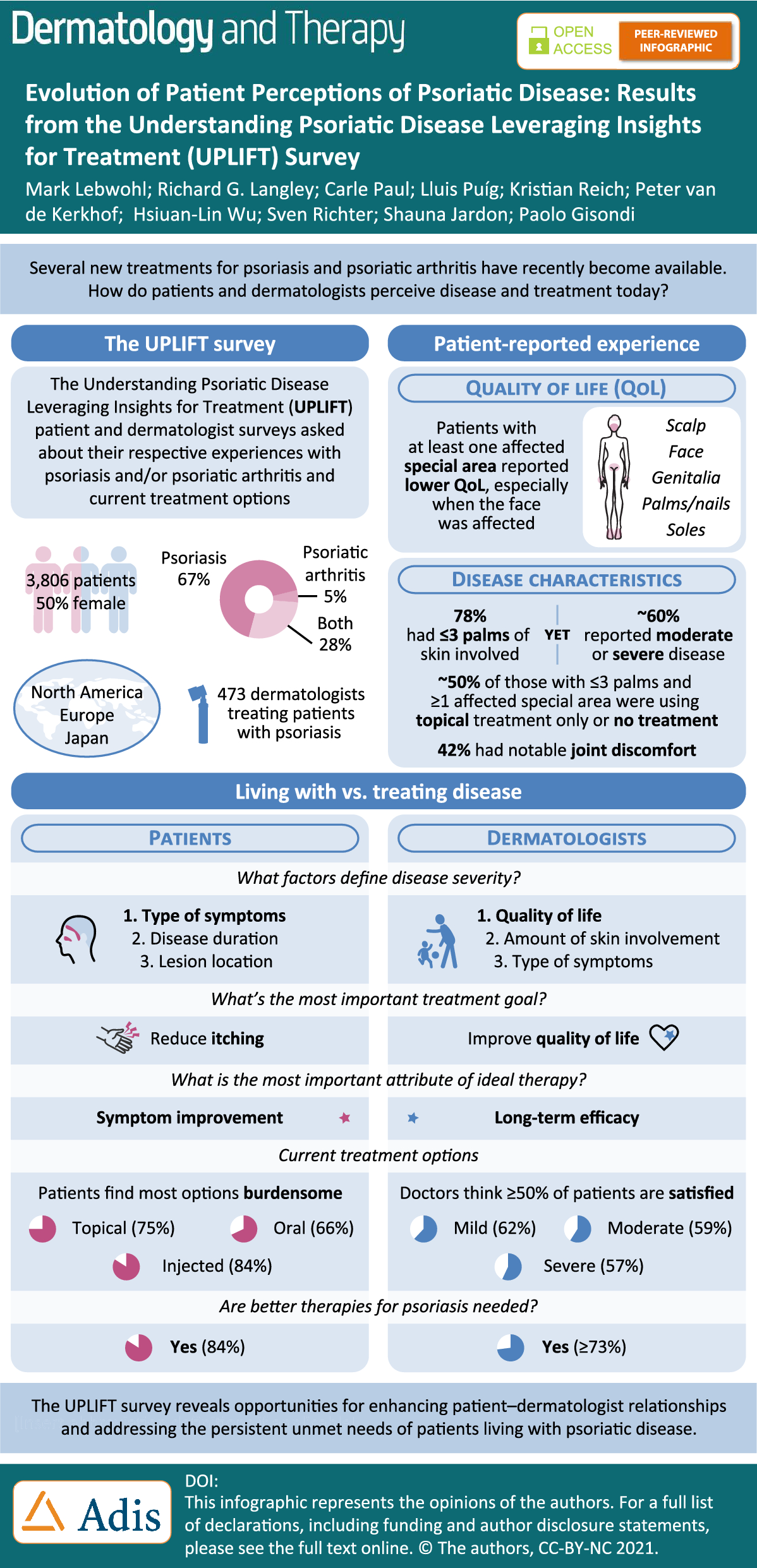
The treatment of psoriatic arthritis is multifaceted, aiming to control symptoms, prevent joint damage, and improve overall quality of life. Treatment options can be broadly categorized into conventional therapies, biologic agents, and emerging targeted treatments.
Conventional Therapies
For many patients, the initial approach involves non-biologic medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These medications, such as ibuprofen or naproxen, help reduce inflammation and relieve pain. They are usually the first line of treatment for mild to moderate symptoms.
- Disease-Modifying Antirheumatic Drugs (DMARDs): Medications like methotrexate have been a mainstay in managing PsA. DMARDs work by slowing down the progression of the disease, reducing joint damage, and controlling systemic inflammation.
While these treatments can be effective, they may not be sufficient for all patients—especially those with more severe or rapidly progressing disease. For further details on conventional management strategies, resources like Central Texas Rheumatology offer practical insights into how these therapies are applied in clinical settings.
Biologic Therapies and Targeted Treatments
Over the past two decades, the treatment landscape for psoriatic arthritis has evolved dramatically with the introduction of biologic therapies. These drugs are designed to specifically target and neutralize the inflammatory cytokines that drive the disease. Key biologic treatments include:
- Anti-TNF Agents: Drugs such as adalimumab, etanercept, and infliximab block tumor necrosis factor-alpha (TNF-α). These agents have demonstrated significant efficacy in reducing both joint and skin symptoms. However, while they often provide rapid relief, some patients may experience diminishing responses over time.
- IL-17 Inhibitors: Medications like secukinumab and ixekizumab target interleukin-17, a cytokine heavily involved in the inflammatory process. They have been shown to significantly improve skin clearance and joint function.
- IL-23 Inhibitors: Agents such as guselkumab and risankizumab specifically target interleukin-23. These drugs help modulate the immune response more precisely, and studies indicate they may normalize cytokine levels, leading to improved clinical outcomes. Research highlighted in a Springer article demonstrates the evolving role of IL-23 inhibitors in achieving skin clearance and reducing joint inflammation.
- JAK Inhibitors: A newer class of medications, including tofacitinib and upadacitinib, works by inhibiting Janus kinase (JAK) pathways that are pivotal in the inflammatory cascade. These treatments offer an alternative for patients who may not respond adequately to biologics.
Biologic therapies are typically reserved for patients with moderate to severe disease or those who do not respond well to conventional DMARDs. They offer the advantage of targeted action, which often results in improved symptom control and a reduced rate of joint damage. However, these treatments may come with higher costs and the need for regular monitoring to manage potential side effects.
Advanced and Emerging Treatment Modalities
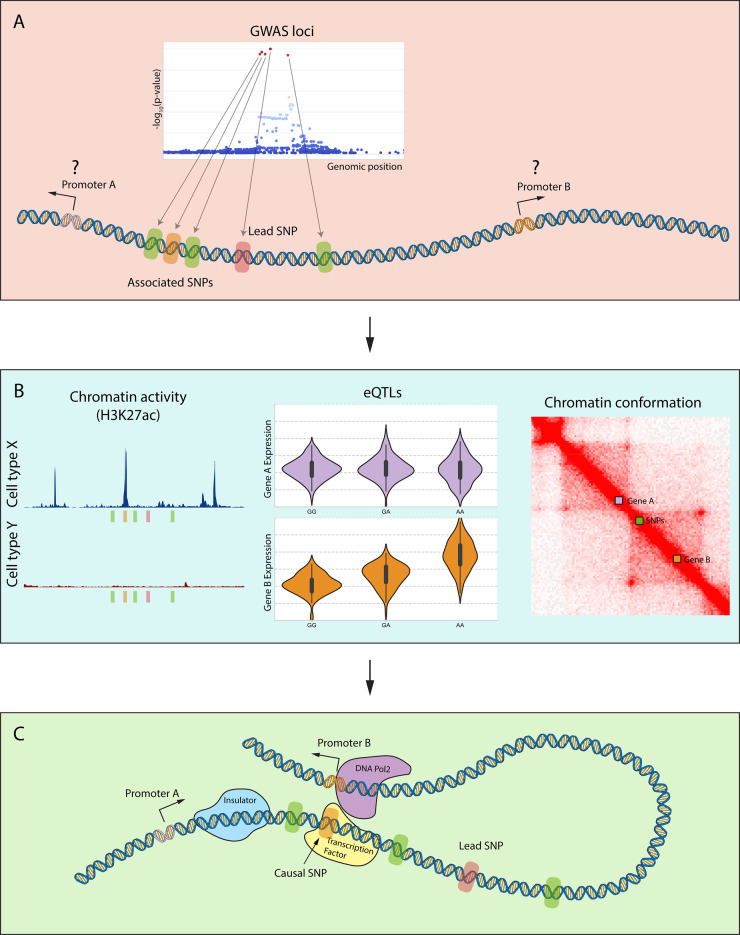
Ongoing research continues to refine our understanding of psoriatic arthritis at the molecular level, leading to innovative approaches in treatment:
- Functional Genomics and Biomarkers: Advanced studies are using genomic tools to identify specific genetic markers and pathways involved in PsA. For example, chromatin conformation analysis helps reveal how genetic variants in non-coding regions affect gene regulation in immune cells. Such research aims to uncover new therapeutic targets and develop personalized medicine approaches. The study details how functional genomics is advancing the understanding of psoriatic arthritis pathogenesis.
- Combination Therapies: In some cases, combining conventional DMARDs with biologics or JAK inhibitors may provide synergistic benefits, leading to better disease control. The choice of combination therapy is highly personalized, taking into account the severity of joint involvement and skin symptoms.
- Personalized Medicine: With the advent of precision medicine, the future of PsA treatment is likely to involve tailoring therapies based on individual genetic profiles and disease characteristics. This approach could help optimize treatment outcomes and minimize unnecessary side effects.
Lifestyle Modifications and Complementary Therapies
While medications play a central role in managing psoriatic arthritis, lifestyle modifications are equally important in maintaining overall health and reducing disease impact. Patients are encouraged to adopt strategies that include:
- Regular Exercise: Low-impact activities such as swimming, walking, or cycling can improve joint mobility, reduce stiffness, and boost overall fitness. Exercise also helps manage weight, which is crucial as obesity is linked to more severe disease.
- Physical Therapy: Targeted exercises and therapies can strengthen the muscles surrounding affected joints, providing better support and reducing pain.
- Stress Management: Techniques such as mindfulness, meditation, and yoga can help reduce stress, which is known to exacerbate inflammatory conditions.
- Dietary Adjustments: A balanced diet rich in anti-inflammatory foods (such as fruits, vegetables, and omega-3 fatty acids) may help control systemic inflammation.
Complementary therapies, including acupuncture and massage, are also increasingly recognized for their role in alleviating pain and improving quality of life. For practical tips and patient-centered strategies, the Saint Luke’s resource provides valuable advice on incorporating lifestyle changes into a comprehensive treatment plan.
The Importance of Early Diagnosis and Intervention
Early detection of psoriatic arthritis is critical to prevent irreversible joint damage and preserve mobility. Studies have shown that patients who receive prompt treatment tend to experience better long-term outcomes. Screening tools, regular check-ups, and open communication with healthcare providers are essential components of early intervention strategies. For instance, awareness of subtle signs such as nail changes or mild joint stiffness can prompt further evaluation and timely treatment.
Patients are encouraged to work closely with rheumatologists—specialists in joint diseases—to establish a treatment plan that is both aggressive enough to control inflammation and tailored to their individual needs. The Franciscan Health blog emphasizes that early diagnosis and consistent treatment can make a significant difference in managing the chronic nature of the disease.
Managing a Chronic Condition: Long-Term Treatment Strategies
Living with psoriatic arthritis requires a long-term commitment to managing symptoms and preventing disease progression. This chronic condition may involve periods of remission and flare-ups, making continuous monitoring and treatment adjustments essential. Some key long-term management strategies include:
- Regular Monitoring: Periodic evaluations through physical exams, imaging studies, and laboratory tests help track disease progression and adjust treatment plans as necessary.
- Patient Education: Staying informed about the latest treatment options and self-care strategies empowers patients to take an active role in managing their condition.
- Multidisciplinary Care: Effective management of PsA often involves a team of healthcare professionals, including rheumatologists, dermatologists, physical therapists, and primary care providers. This collaborative approach ensures that both joint and skin symptoms are addressed comprehensively.
For those seeking specialized care, resources like Central Texas Rheumatology offer personalized treatment plans and expert guidance tailored to individual patient needs.
Advances in Research and Future Directions
The field of psoriatic arthritis treatment is dynamic, with ongoing research aimed at uncovering new therapeutic targets and refining existing treatment approaches. Recent advances in molecular biology and immunology have provided deeper insights into the complex interplay between genetic factors and immune system dysregulation in PsA. Key research areas include:
- Biomarker Identification: Researchers are actively working to identify biomarkers that predict treatment response and disease progression. These biomarkers could pave the way for personalized medicine, where therapies are tailored to the specific inflammatory profile of each patient.
- Novel Drug Targets: Studies investigating the role of inflammatory cytokines have led to the development of novel agents that more precisely target the IL-23/IL-17 pathway. For example, research published in the BMJ journal has provided new insights into how differential expression of IL-23 in skin versus joint tissues may influence treatment outcomes.
- Functional Genomics: By using genomic and epigenomic tools, scientists are beginning to unravel the mechanisms by which genetic variations contribute to PsA. This research not only enhances the understanding of disease pathogenesis but also guides the development of innovative therapies designed to halt disease progression before irreversible joint damage occurs.
The future of psoriatic arthritis treatment looks promising, with the potential for more targeted therapies that offer greater efficacy and fewer side effects. As our understanding of the disease deepens, patients can look forward to more personalized treatment regimens that address their unique clinical profiles.
Practical Considerations When Choosing a Treatment Plan
When deciding on a treatment plan for psoriatic arthritis, several factors need to be taken into account:
- Disease Severity and Symptom Profile: The choice of therapy often depends on the severity of joint involvement, skin symptoms, and the overall impact on quality of life. Some patients may respond well to conventional treatments, while others require the precision of biologic or targeted therapies.
- Side Effect Profiles: All medications have potential side effects. It is important for patients to discuss the benefits and risks of each treatment option with their healthcare provider.
- Cost and Accessibility: Biologic therapies, though effective, can be costly. Insurance coverage and availability of patient assistance programs may influence treatment decisions.
- Lifestyle and Personal Preferences: A holistic treatment plan should consider the patient’s lifestyle, preferences, and any comorbid conditions. For instance, those with a busy schedule may prefer medications that require less frequent dosing, while others may focus on treatments that offer rapid relief from pain and swelling.
Patients are advised to remain proactive in their care by asking questions, seeking second opinions if necessary, and staying updated on the latest research. Empowered patients often find that a well-informed approach leads to better management of their condition.
Integrating Complementary Therapies
In addition to pharmacological treatments, complementary therapies can play a supportive role in managing psoriatic arthritis. These approaches include:
- Physical Therapy: Customized exercise programs not only improve joint function but also enhance overall mobility. Working with a physical therapist can help design an exercise regimen that minimizes joint strain while promoting strength and flexibility.
- Occupational Therapy: This form of therapy focuses on adapting daily activities to reduce joint stress and maintain independence. Adaptive tools and techniques can be integrated into everyday routines.
- Mind-Body Practices: Stress management techniques such as yoga, meditation, and mindfulness have been shown to reduce inflammation and improve overall well-being. A calmer mind often contributes to a more manageable physical state.
- Diet and Nutrition: While no specific diet cures psoriatic arthritis, a balanced diet rich in antioxidants and anti-inflammatory foods may help reduce systemic inflammation. Maintaining a healthy weight is especially important, as obesity can exacerbate joint pain and hinder mobility.
These supportive therapies not only complement conventional treatments but also empower patients to take an active role in managing their condition.
Conclusion
Understanding psoriatic arthritis and its treatments involves a multifaceted exploration of the disease from it’s genetic and immunological roots to the wide range of therapeutic options available today. While conventional treatments like NSAIDs and DMARDs provide a foundation for managing inflammation and pain, the advent of biologics and targeted therapies has revolutionized the approach to care. Advances in research continue to unveil new insights, promising more personalized and effective treatments in the future.
Living with psoriatic arthritis may present challenges, but with the right combination of treatments, ongoing research, and a proactive approach to health, it is possible to lead a fulfilling and active life. Always consult with a healthcare professional to determine the best treatment strategy for individual needs, and remain open to new therapies as they emerge in this dynamic field.
This guide is intended to serve as a comprehensive resource to help demystify psoriatic arthritis treatments and provide practical insights for long-term management. By combining robust scientific research with patient-focused advice, it is hoped that those affected by PsA can feel empowered and informed in their journey toward better health.
The content provided is not a substitute for professional medical advice, diagnosis, or treatment. Please consult your healthcare provider with any questions you may have regarding your condition.
Sources: